|
|
||
|
||
|
Privacy Policy | Editorial Policy | Profit Policy | Join the Association | List of Members | Contact us | Index | Links |
||
|
Back Go to page: 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Forward
|
||
|
Health and Life Style. |
||
| Veterans and Veterans Families Counselling Service (VVCS) can be reached 24 hours a day across Australia for crisis support and free and confidential counselling. Phone 1800 011 046. VVCS is a service founded by Vietnam Veterans. |
||
|
|
||
|
Choking.
Choking occurs when a foreign object becomes lodged in the throat or windpipe, blocking the flow of air. In adults, a piece of food often is the culprit whereas young children often swallow small objects. Because choking cuts off oxygen to the brain, administering first aid as quickly as possible is crucial.
The universal sign for choking is hands clutched to the throat. If the person doesn't give the signal, look for these indications:
If choking is occurring, the Red Cross recommends a "five-and-five" approach to delivering first aid:
It's OK not to use back blows, if you haven't learned the technique. Both approaches are acceptable.
To perform abdominal thrusts (Heimlich maneuver) on someone else:
If you're the only rescuer, perform back blows and abdominal thrusts before calling 000 for help. If another person is available, have that person call for help while you perform first aid.
If the person becomes unconscious, perform standard CPR with chest compressions and rescue breaths.
To perform abdominal thrusts (Heimlich maneuver) on yourself:
First, if you're alone and choking, call 000 immediately. Then, although you'll be unable to effectively deliver back blows to yourself, you can still perform abdominal thrusts to dislodge the item.
To clear the airway of a pregnant woman or obese person:
To clear the airway of an unconscious person:
To clear the airway of a choking infant younger than age 1:
If the child is older than age 1, give abdominal thrusts only.
To prepare yourself for these situations, learn the Heimlich maneuver and CPR in a certified first-aid training course.
Mozzie Bites.
Avoid and exclude mosquitoes
Limit exposure to mosquitoes by:
The most effective insect repellents include one of three active ingredients:
These repellents temporarily repel mosquitoes and ticks. DEET may offer longer lasting protection. Whichever product you choose, read the label before you apply it. If you're using a spray repellent, apply it outdoors and away from food.
If you're also using sunscreen, put it on first, about 20 minutes before applying the repellent. Avoid products that combine sunscreen and repellent, because you'll likely need to reapply sunscreen more often than repellent. And it's better to use only as much repellent as you need.
Used according to package directions, these products are generally safe for children and adults, with a few exceptions:
Treat clothing and outdoor gear
Permethrin is an insecticide and insect repellent used for additional protection. This product is applied to clothing and outdoor gear, not skin. Check the product label for specific application instructions. Some sporting goods stores sell clothing pretreated with permethrin.
Use protective clothing and gear.
Weather permitting, wear:
Take preventive medication.
If you tend to have large or severe reactions to mosquito bites (skeeter syndrome), consider taking a nondrowsy, nonprescription antihistamine when you know you'll be exposed to mosquitoes.
Reduce mosquitoes around your home.
Eliminate standing water, which mosquitoes need to breed. To keep your house and yard free of mosquito pools:
|
||
|
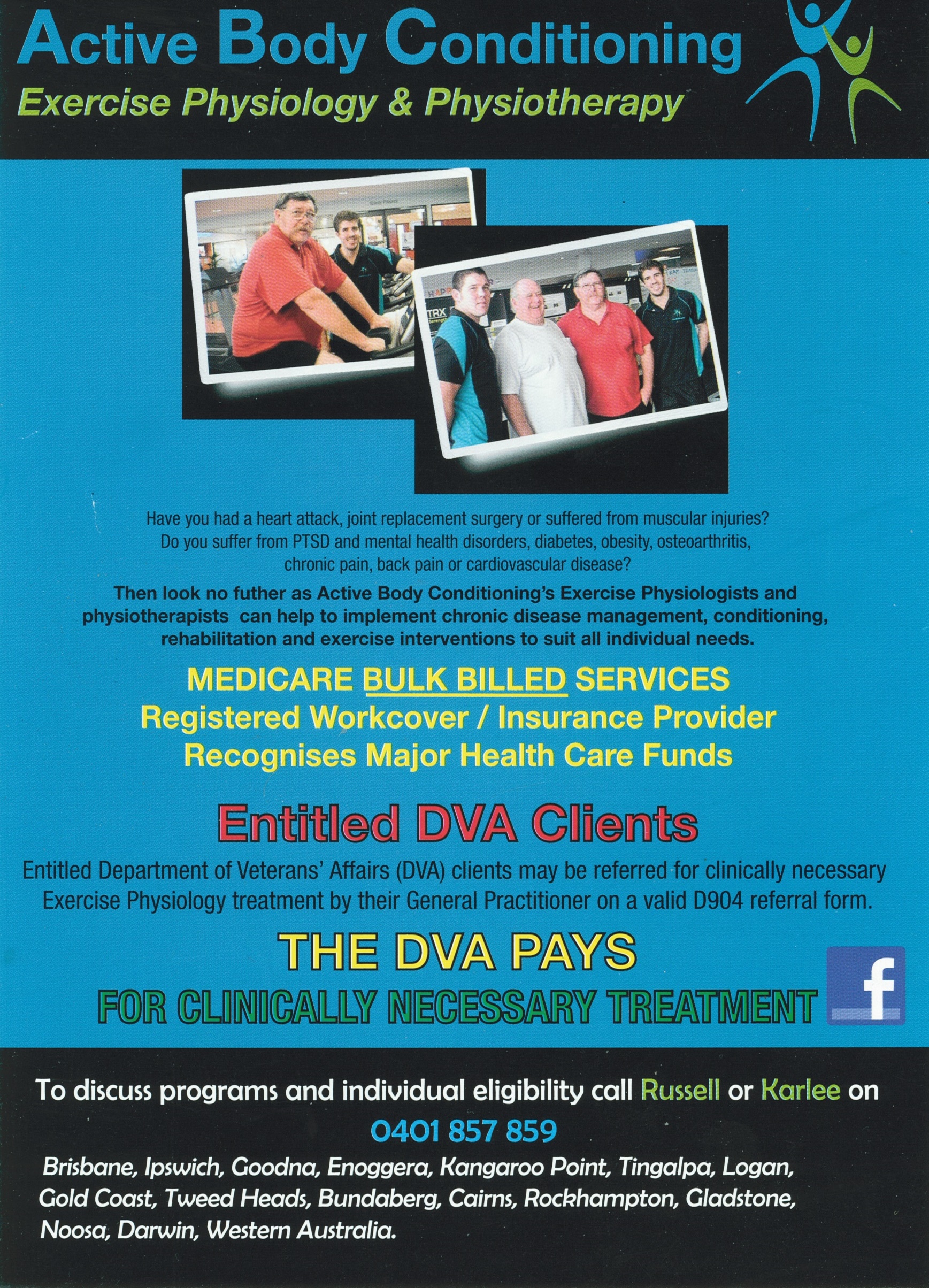
Safeguarding veterans’ pharmaceutical benefits.
On 1 July 2017 Minister for Veterans’ Affairs Dan Tehan announced additional funding to ensure Department of Veterans’ Affairs (DVA) clients would continue to have access to pharmaceuticals through the Repatriation Pharmaceutical Benefits Scheme (RPBS). “From 1 July 2017, the Australian Government will provide $663,000 in additional funding over five years for 35 pharmaceutical items,” said Mr Tehan. “The funding will safeguard the availability of 34 items, one new listing and the addition of five generic brands.” The generic brands treat insomnia, skin cancer, fungal mouth infections, diarrhoea and assist in preserving bone mineral density.
Microdacyn, a sterile irrigation solution that assists in the treatment of wounds and is applied as a topical wound healing agent, will be added to the RPBS. These additions reflect new therapies becoming available, generic brands coming onto the market and pharmaceutical sponsors seeking to vary prices. “The Australian Government is continuously exploring ways to provide more pharmaceutical options at a lower cost to veterans,” Mr Tehan said. “Australia will always be grateful to our veterans for the service they have provided to the nation.
Ensuring access to affordable medications is one way the Government demonstrates our appreciation.”
When should I take calcium supplements? Does the timing matter?
Yes. Three factors determine when you should take calcium supplements:
It's also a good idea to take your calcium supplements at a different time from your multivitamin or an iron-rich meal. Calcium may not be absorbed as well if it's taken at the same time as iron, zinc or magnesium.
If you still aren't sure about the best time to take calcium supplements, check with your doctor or pharmacist for guidance.
|
||
|
|
||
|
|
||
|
How CPAP controls sleep apnea.
Continuous positive airway pressure (CPAP) is a treatment option for sleep apnea. As you sleep, CPAP provides air at a pressure just high enough to prevent the collapse of your airway. The pressurized air is provided through a mask that seals with your mouth or nose. This allows you to breathe without much effort and sleep without waking up.
The CPAP machine doesn't breathe for you. You can breathe in and out normally on your own.
Some people require different pressures during the inhale and exhale cycle to help them breathe more normally or comfortably.
A variety of masks are available. If one type of mask or machine isn't comfortable, ask your doctor for suggestions about other options for you.
Click HERE to see a video explaining it.
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
Pet therapy: Man's best friend as healer.
Animal-assisted therapy can help healing and lessen depression and fatigue.
Is medicine going to the dogs? Yes, but in a good way. Pet therapy is gaining fans in health care and beyond. Find out what's behind this growing trend.
What is pet therapy?
Pet therapy is a broad term that includes animal-assisted therapy and other animal-assisted activities. Animal-assisted therapy is a growing field that uses dogs or other animals to help people recover from or better cope with health problems, such as heart disease, cancer and mental health disorders.
Animal-assisted activities, on the other hand, have a more general purpose, such as providing comfort and enjoyment for nursing home residents.
How does animal-assisted therapy work?
Imagine you're in the hospital. Your doctor mentions the hospital's animal-assisted therapy program and asks if you'd be interested. You say yes, and your doctor arranges for someone to tell you more about the program. Soon after that, an assistance dog and its handler visit your hospital room. They stay for 10 or 15 minutes. You're invited to pet the dog and ask the handler questions.
After the visit, you realize you're smiling. And you feel a little less tired and a bit more optimistic. You can't wait to tell your family all about that charming canine. In fact, you're already looking forward to the dog's next visit.
Who can benefit from animal-assisted therapy?
Animal-assisted therapy can significantly reduce pain, anxiety, depression and fatigue in people with a range of health problems:
And it's not only the ill person who reaps the benefits. Family members and friends who sit in on animal visits say they feel better too. Animals also can be taught to reinforce rehabilitative behaviours in patients, such as throwing a ball or walking.
Pet therapy is also being used in nonmedical settings, such as universities and community programs to help people deal with anxiety and stress.
Does pet therapy have risks?
The biggest concern, particularly in hospitals, is safety and sanitation. Most hospitals and other facilities that use pet therapy have stringent rules to ensure that the animals are clean, vaccinated, well-trained and screened for appropriate behaviour.
It's also important to note that the Centres for Disease Control and Prevention has never received a report of infection from animal-assisted therapy.
Animal-assisted therapy in action.
More than a dozen registered therapy dogs are part of Mayo Clinic's Caring Canines program in the US. They make regular visit to various hospital departments and even make special visits on request. The dogs are a welcome distraction and help reduce the stress and anxiety that can accompany hospital visits.
|
||
|
|
||
|
|
||
|
|
||
|
|