|
|
||
|
||
|
Privacy Policy | Editorial Policy | Profit Policy | Join the Association | List of Members | Contact us | Index | Links |
||
|
Back Go to page: 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Forward |
||
| Veterans and Veterans Families Counselling Service (VVCS) can be reached 24 hours a day across Australia, for crisis support and free and confidential counseling phone 1800 011 046. VVCS is a service founded by Vietnam Veterans.
|
||
|
Health and Life-style. |
||
|
|
||
|
Contents
Confusion over who can acess weight loss drug. Does beer cause the pot belly? Does being drunk harm your body? What causes the stitch when running?
|
||
|
|
||
|
Will coffee dehydrate you?
Everyone knows water is the best way to stay hydrated and you might have heard that it’s important to drink it with your coffee in the morning to prevent dehydration. But is that actually true?
Does coffee dehydrate you? The answer isn’t straightforward, but if you’re drinking coffee within recommended amounts, you’re not likely to become dehydrated. The whole coffee consumption leads to dehydration idea likely gets blown out of proportion because the beverage is a diuretic. Essentially, it can cause your body to make more urine than usual because it increases blood flow to the kidneys. If you’re peeing more, you’ll get dehydrated, right? Well, not necessarily.
In moderate servings, coffee can actually hydrate you, and even if you drink quite a bit of caffeine (up to 300mg), it’s still unlikely to cause an obvious diuretic effect. Essentially, coffee might cause you to pee more because it’s a diuretic, but that additional urine output is likely not enough to dehydrate you.
Does that mean you should forgo a morning glass of water? Probably not. Keeping your body hydrated is still an important part of overall health, but you don’t need to toss back four glasses of it to “keep up” with your coffee intake. As long as you’re drinking caffeine moderately, you should be just fine.
If one of your new year’s resolutions was to drink more water, go ahead, but you don’t need to give up your coffee in the name of hydration.
Confusion over who can access weight-loss drug.
Natasha Yates, Assistant Professor, General Practice, Bond University
Semaglutide, sold in the forms of Ozempic and Wegovy, shot into public consciousness as an effective weight-loss medication last year, thanks to spruiking from social media influencers and people such as Elon Musk. The unexpected increase in demand for the drug for weight loss has caused a worldwide shortage. Producing the drug, delivered as a weekly self-administered injection, involves a unique manufacturing set-up, so it will take some time to re-establish a global supply. It’s expected back in Australia at the end of March.
Semaglutide (in the form of Ozempic) is an effective medication in managing type 2 diabetes, and the shortage has left some people with diabetes struggling to find pharmacies with their treatment in stock. For many people with diabetes, Ozempic has controlled their blood sugar (and often also helped them lose weight) more effectively than other medications. Due to the shortage of Ozempic, Australian GPs have been advised against prescribing it to treat obesity, however, semaglutide in the form of Wegovy is designed specifically for weight loss. US and Australian regulators have recently approved Wegovy for that purpose, though it hasn’t been available for use in Australia to date.
When the shortage is resolved and semaglutide is once again available in Australia for those with diabetes, it’s unclear who will be able to access it for weight loss. Patients and doctors are also asking how much they will pay, and what role it will play in managing obesity.
How does it work?
Semaglutide works in several ways, including increasing feelings of fullness by acting on appetite centres in the brain and slowing stomach emptying. It affects the secretion of insulin and glucagon, which is why it is so effective in diabetes. It also reduces the risk of heart attacks and strokes. Other weight-loss drugs in the past have reduced weight but increased the risk of dying from a heart attack, which made them overall too dangerous.
Studies show semaglutide helps 66 to 84 per cent of people who use the drug to lose weight, making it more effective than other drugs on the market. After two years, patients using it still benefit by not regaining their lost weight, but only if they are still taking the drug. Disappointingly, once stopped, patients notice a gradual regain of up to two-thirds of the weight they lost. So essentially, semaglutide works only while taking it – it ‘manages’ but does not ‘cure’.
Semaglutide is meant to be an add-on, not a replacement, for exercise and a healthy diet.
Research on the medication has always been done in conjunction with a healthy diet and exercise, as that is considered best practice. So we don’t know what happens if you just take the medication without also starting or maintaining a healthy lifestyle. We do know exercise is key to keeping weight off over time.
What are the side-effects?
Semaglutide can cause nausea, bloating, constipation and diarrhoea. Questions have been raised around the risk of pancreatitis, and thyroid and pancreatic cancers. So far the research is reassuring, however these are all rare, so it’s unlikely we will know if there is any significant increase for some years to come.
How much does it cost?
One of the biggest barriers to semaglutide for weight loss is the cost. Although patients spend less on food while taking it, in 2022 (when it was more easily available in Australia) it cost around $130 a month. It could be pricier once supply issues are fixed, because the manufacturer, Novo Nordisk, is spending millions of dollars building new facilities to meet the increased demand.
In the US, prices are already over US$1000 a month unless covered by insurance. Australians with diabetes will continue to be able to access the drug on the Pharmaceutical Benefits Scheme (PBS) for the usual cost of a script, however, if used for obesity, it would be on a private prescription, so the cost is still unknown.
Obesity is more common among people with lower incomes, so from a public health perspective, those who would benefit the most may least afford it. This lack of equity must be wrestled with if this medication becomes widely used for obesity management. Subsidising on the PBS for weight loss is one option.
What are the downsides?
A serious concern is the potential for semaglutide to be used by people who are not obese, particularly those with eating disorders. Because it suppresses appetite, it could enable people to starve themselves in an unhealthy way.
Obesity is defined as a body mass index (BMI) of over 30, and overweight is BMI of 25-30, yet there are reports of people with BMIs less than 25 using it to drop “just a bit of weight”. The psychological and social pressure to be thin is a powerful driver, particularly in a society that frequently stigmatises obesity. People may see semaglutide as a way of ‘treating’ their body image issues.
Another concern is the impact on enjoying food. Patients feel full after just a few bites, making meals with friends awkward, and sometimes limiting their social life.
Why have doctors prescribed it for weight loss?
First-line obesity management should always be lifestyle interventions: improving your diet and getting more exercise, with the help of a multidisciplinary team, but when this is insufficient, patients’ options are limited. The most effective is bariatric surgery. Although surgery is generally well tolerated, it is an irreversible lifelong change.
Once the semaglutide access issues are resolved,
Australian regulators should seek input from the community and from
doctors, and think carefully about the role the drug should play in
Australia’s management of obesity and weight loss. In addition to
equitable access and protection for those with body image issues, we
will need clear, evidence-based guidelines that consider the
psychological and social impact of the drug.
What causes Side Stitches when running?
A side stitch, also known as a side ache or a cramp is an intense stabbing pain in your side that occurs during exercise. Sometimes the pain goes away during your workout and sometimes it sticks around until you stop exercising altogether. Whatever the case, side stitches are frustrating. But what causes side stitches, and is here a way to prevent them? Here’s what to know.
What Causes a Side Stitch?
About 70 percent of runners experience at least one instance of exercise-related transient abdominal pain (ETAP) each year. The condition seems to be most common in runners, although bikers, swimmers, and other exercise lovers also report incidences of it.
As common as side stitches are, scientists still aren’t sure exactly what causes them. Some believe it has to do with the overuse of the diaphragm muscle, which is crucial to the breathing process and is therefore heavily relied upon by runners. Repeatedly hitting one’s feet against the ground while the diaphragm is fully expanded may cause the muscle to spasm and cramp.
Other scientists believe the condition may be caused when organs start to bounce around during intense exercise, however, this theory doesn’t hold much weight though, because bikers and swimmers often maintain good posture and still get side stitches.
More theories as to what causes side stitches include having an increased curvature of the spine, drinking sugary beverages before exercising, skipping warmups before exercising, and employing improper breathing techniques. But the most likely explanation points to the lining of the abdominal and pelvic cavity known as the peritoneum. This membrane helps to support all the organs in the body. Normally, fluid between the separate layers ensures that they don’t rub against each other, but after a person eats a large meal, the layers expand and press against each other and, when the body is dehydrated, less fluid is available between the layers.
Ultimately, both of these factors may contribute to the layers rubbing against each other, which causes the sharp pain associated with a side stitch. Many athletes also report shoulder pain during a side stitch, which fits in with this theory because when the abdominal lining is irritated, pain may be localized in other parts of the body.
How Do You Treat Side Stitches?
The easiest way to treat a side stitch is to stop exercising until it passes. The pain usually subsides within minutes after the body relaxes, however, if you must keep exercising (if you’re in a competition, for example), breathe deeply and exhale slowly. Regulating your breathing can help relax the body and thus may limit uncomfortable rubbing.
How Do You Prevent Side Stitches?
Preventing side stitches may take some trial and error on your part, however, there are some definite no-nos. Don’t eat for at least two or three hours before working out, although you may need to extend this time if you still experience problems within this timeframe. Avoid high-fiber and high-fat foods before exercising. Don’t drink sugary beverages either before or during your workout. Take note of what you eat and drink before running or biking and use that information to make adjustments until you find something that works for you.
|
||
|
|
||
|
|
||
|
Five sunburn myths you need to stop believing.
Whether you’re a sun worshipper who welcomes every heatwave with open arms, or you prefer to stay in the shade all year round, sometimes it’s hard to to avoid catching the sun, but a touch of prickly pink skin at the end of the day isn’t really going to make a difference, is it?
Wrong – experts suggest even mild sunburn can put you at risk of skin cancer and that’s not the only mistake many people make when it comes to sun protection. Following are five common misconceptions about sunburn, and what you need to do to stay safe.
1. The odd sunburn doesn’t make a difference.
This is something you hear a lot but unfortunately, it’s just not true. Damage to our skin from the sun is the number one cause of melanoma, the most serious type of skin cancer and skin damage from the sun builds up over time, it doesn’t go away after the burn fades. Every burn counts, but this also means every time you protect yourself also counts. This is even more important for children. According to the Skin Cancer Foundation (skincancer.org), “even one blistering sunburn in childhood or adolescence more than doubles your chances of developing melanoma later in life”.
2. You have to go red before you go brown.
Want to get a gorgeous, golden brown tan this summer? Your skin doesn’t need to turn red first. This is one of the biggest myths in sun protection and it contributes to skin damage and skin cancer cases.
“The fact is that as soon as the skin reddens, it’s in trauma. A ‘trauma tan’ occurs from inadequate protection where the skin appears to tan more quickly, but hasn’t – it has burned. This only ensures that the skin peels, leaving the skin tan-less in days.”
To tan safely, gradually build up your time in the sun and use a higher SPF sunblock. Use high UVA and UVB filter SPF, a minimum of SPF30 with a UVA filter of more than 90 per cent will protect the skin and still allow you to tan, just more slowly and minimising long-term damage and peeling.
3. A tan will protect you from sunburn.
Even once you’ve started to tan, your skin is still at risk. People with naturally darker skin tones have a lower risk of skin cancer than people with lighter skin tones, although everyone is at risk, but going out and getting a base tan before your holiday doesn’t provide the extra protection you might think.
4. All body parts are created equal when it comes to sunscreen.
Burning, overexposure to UVB rays, tends to happen where the skin is closer to the bone structure, and especially where the part of the body faces directly the sun’s rays which is why you often see pink patches in the same places after a day in the sun. Take extra care in the following areas, tops of feet, shoulders, for ladies - the top of the breast area, top of the scalp and the nose. Other common sites include the scalp or parting, sides of the face and ears, areas around swimwear such as straps, and shorts that might move or rise up through the day. A good idea is to do your sun cream while naked then any movement in straps, shorts won’t suddenly bare unprotected skin to the sun’s rays.
5. You can’t get burnt in the shade.
Effective shade can provide protection from the sun’s UV rays, but we can still get burnt in the shade. Shade materials with holes or gaps can allow penetration by UV radiation. The same rule applies for tree shade, with denser foliage and wider canopies providing better protection than trees with sparse foliage and dappled sunlight. Reflected UV radiation is another factor that means you’re not always safe in the shade. The sun’s rays reflect from light-coloured surfaces and can bounce back under shade. Light surfaces, such as concrete, light-coloured paint or metallic surfaces, reflect more than dark ones. Sand can reflect as much as 25 per cent of UV radiation. This means if you’re sitting under a beach umbrella, UV radiation can still damage your skin, even though you feel like you’re covered in the shade.
|
||
|
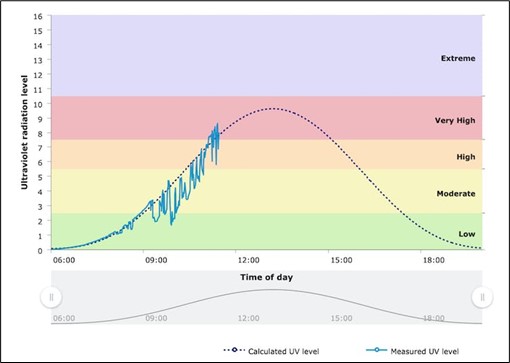
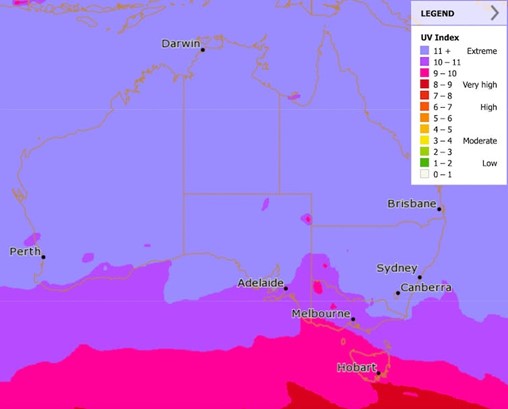
What is the UV index?
You’ve probably seen the UV index in the day’s weather forecast, and you know it tells you when you need to cover up and wear sunscreen. But where does that number come from?
It is produced at the Australian Radiation Protection and Nuclear Safety Agency (ARPANSA).
It’s their job to help keep Australia safe from all kinds of radiation, and that doesn’t just mean nuclear reactors and mobile phone signals – it also means radiation from the sun. Australia has one of the highest rates of skin cancer in the world, accounting for about 80 per cent of cancers diagnosed in Australia each year. Most skin cancers are caused by exposure to UV radiation from the sun.
What is the UV index?
The UV index tells you how much ultraviolet radiation is around at ground level on a given day, and its potential to harm your skin.
UV radiation is a component of sunlight that can cause tanning and sunburn in the short term. In the longer term, too much exposure to UV can cause cataracts and skin cancer. In 2002, the World Health Organization (WHO) devised the UV index in an effort to make people around the world more aware of the risks. The index boils down several factors into a single number that gives you an idea of how careful you need to be in the sun. A score of 1 or 2 is low, 3–5 is moderate, 6 or 7 is high, 8–10 is very high, and 11 and above is extreme.
What is UV radiation?
The sun showers the earth with light at a huge spectrum of different wavelengths and each wavelength can have a slightly different effect on human skin. An important part of the spectrum is ultraviolet or UV radiation: light with wavelengths too short for our eyes to see, from around 400 nanometres to 10 nanometres. (A nanometre a metric is a unit of length equal to one thousand-millionth of a metre.)
There are two important kinds of UV radiation: UV-A, with wavelengths from 400–315 nanometres, and UV-B with wavelengths from 315–280 nanometres. (Shorter wavelengths are called UV-C, but are mainly blocked by the atmosphere so we don’t need to worry about it.)
UV-A and UV-B both contribute to skin damage, ageing and skin cancer. But UV-B is the more dangerous: it is the major cause of sunburn, cataracts and skin cancer.
How is the UV index calculated?
The UV index takes into account how much UV radiation of different wavelengths is around and how each of those wavelengths affects our skin. ARPANSA has a network of sensors around Australia measuring sunlight at different wavelengths to determine the UV index, with the information available online in real time.
|
||
|
|
||
|
This data is combined with other information about location, cloud cover and atmospheric conditions to produce maps and forecasts of the UV index for the whole country.
How are UV levels different around the world?
The UV index you see reported is usually the daily maximum – that’s the highest it will be all day. How high it gets depends on lots of factors, including your location, the time of year, the amount of cloud cover, and ozone and pollution in the atmosphere. The index tends to be higher closer to the equator and at high altitudes, as the sunlight has to pass through less air before it reaches the ground.
People often experience the sun in Australia as particularly harsh, compared with places in North America or Europe. In a British summer, for example, the maximum UV index might be between 6 and 8. In an Australian summer it can range from 10 to 14. There are a few reasons for this. One is that Australia’s cities are closer to the equator than many big cities in Europe and North America. Another is that the earth is very slightly closer to the sun in the southern hemisphere’s summer than the northern summer, meaning the sunlight is a few per cent brighter.
A third reason is the ‘hole’ in the ozone layer. The layer of ozone in the upper atmosphere, which absorbs some UV-B, is thinner towards the South Pole. This was caused by the use of chemicals called chlorofluorocarbons or CFCs, and it has been improving since they were banned by an international agreement in 1987. And finally, the air in Australia generally has less smoke, dust and other small particle pollution than many places in the northern hemisphere. While this makes the air nicer to breathe, pollution does absorb or block some UV radiation.
Is UV changing over time?
We know UV levels have increased in recent decades. In Australia, a study in 2011 found the average UV index had increased by 2–6 per cent between the 1970s and the period 1990–2009, due to depletion of the ozone layer. A NASA study found similar results for 1979–2008. It’s harder to say what will happen in the future, as there are several uncertain factors.
It is expected the ozone layer will slowly recover from the impact of CFCs, which is likely to reduce UV levels, however, it is also expected less fossil fuel will be burned, which would mean less air pollution and higher UV levels. On the flip side, we may also have more bushfires due to climate change, which would mean more air pollution and lower UV.
Clouds are also likely to behave differently due to climate change, but we’re not sure exactly how. Researchers in Japan found reductions in clouds and tiny particles in the air are expected to have a bigger impact than the recovery of the ozone layer, which would mean UV levels are likely to go up overall. Regardless of the long-term trends, the daily levels will still be measured and the public will still be advised of the important sun protection times.
Don’t make these sunscreen mistakes.
Everyone knows that slathering on sunscreen is essential during the sunnier months, but how much should you actually use? Can you skip it when it’s cloudy? And do darker skin tones need protecting?
Not knowing the answers to these questions could mean you’re putting your skin and your health at risk. To help ensure you don’t burn this summer, following are some common SPF mistakes and how to avoid them.
1. Not using enough sunscreen.
The easiest way to visualise is via teaspoons. It’s recommended to use half a teaspoon for the face, neck and each arm. Then a full teaspoon for each leg, the front (chest and stomach) and the back. This totals six teaspoons, but if you don’t feel that’s enough then it’s always good practice to add more.
If you’re applying enough, you should restock your sunscreen supply several times each summer.
Research shows most people apply only 25 to 50 per cent of the amount of sunscreen used during testing, which means your actual SPF coverage is about one-third of what’s on the label. In other words, an SPF 30 is only as strong as an SPF 10 if you don’t apply it thoroughly.
2. Not using sunscreen on a cloudy day.
This is the biggest sunscreen myth. Sunscreen should be worn every day. Clouds filter out sunlight but not UV rays, so even on a cloudy day you’re still getting up to 80 per cent of the sun’s harmful effect. If you’re going outside, then you should still cover up; your skin may not burn but it’s still being exposed to long-term risks. The Sun Smart website recommends wearing sunscreen every day that the UV index is higher than three, come rain, hail or shine. The Cancer Council has a free Sun Smart app that gives you live updates on UV levels, a sunscreen calculator and reminders to reapply.
3. Missing spots.
We’re often pretty diligent when it comes to applying sunscreen to the face but it’s easy to miss those pesky hard to reach spots. So, it’s no coincidence that these three often-neglected spots are among the most frequent sites for basal and squamous cell carcinomas, the two most common non-melanoma skin cancers. These commonly missed areas include the scalp, ear, lips, front and back of the neck, backs of hands, and top of the feet. Melanoma, meanwhile, crops up frequently on the backs of women’s legs, another area that is hard to see and reach. Ensure you coat all exposed areas with sunscreen and reapply regularly. Look for lip balms with SPF included and reapply every 90 minutes to two hours.
4. Believing your sunscreen is waterproof.
Waterproof sunscreen doesn’t exist but it is water resistance. This means the product won’t instantly come off the skin when it meets water and is designed for people who will be swimming or heavily perspiring. It is essential to reapply the product straight after coming out of the pool and drying, or regularly whilst perspiring.
5. You rely solely on sunscreen.
Sunscreen is a very important part of sun protection, but it shouldn’t be the only one. We should also avoid prolonged and intense sun exposure (like tanning) whenever possible and wear clothing and accessories to help block the sun. Darker-coloured fabrics with a tight weave and fit offer the most UV protection. The damaging effects of UVA rays still penetrate your skin whilst you are indoors and near a window, therefore, ensure you cover up whilst in the car or seated near the window.
|
||
|
The beer ingredient that could prevent Alzheimer’s
It’s the sort of news that beer lovers would love to hear: Beer could help protect you against Alzheimer’s disease. Given the mostly negative health outcomes usually associated with research into alcoholic drinks, such news would be welcome to lovers of lager and purveyors of pints.
But could it really be true?
The answer is yes – sort of. As is so often the case with scientific research, there are caveats. New research published by the American Chemical Society has found that beer hop compound extracts may inhibit the build-up of amyloid beta proteins in the brain. Amyloid beta proteins have long been pegged as markers for the onset of Alzheimer’s, so anything that inhibits their build-up is likely to be a good thing.
How scientists came to even hypothesise about beer hops as a potential preventer of Alzheimer’s is an interesting story in itself. They started many years ago by studying some natural and synthetic molecules that were able to counteract the early stages of the disease. That led them to wonder if these molecules could perhaps be routinely taken as part of a regular diet. Their studies then focused on the search for bioactive molecules present in food and edible plants and of course, there are many flower hops that come under the umbrella term of ‘edible plants’.
In the new study, the researchers focused on four different hops commonly used in the preparation of beer and herbal tea: Cascade, Saaz, Tettnang and Summit. Of the 42 compounds they identified in the four types, some included compounds linked to reducing blood sugar levels and antioxidant activity. They also analysed the ability of each hop extract to inhibit amyloid beta accumulation, and found that all four could inhibit the build-up of amyloid beta proteins.
One particular type of hop, called Tettnang, which is found in many lagers and light ales, provided especially promising results. The researchers concluded that their results point towards the development of nutraceuticals that may prevent Alzheimer’s. For those who have long been hoping for their regular brew to be classified as a ‘nutraceutical’ (a fancy word for foods that have some type of medicinal or nutritional function) that sounds like great news.
But – and sadly with alcoholic beverages there is almost always a ‘but’ – it’s not that simple. Importantly, the message should not be that drinking hoppy beer can lead to brain-based benefits or prevent Alzheimer’s disease. The benefits of the hops chemicals are likely to be diluted when combined with alcohol and the caloric ingredients found in beer.
The bottom line? Depending on the beer you favour, you may be taking in some compounds that help prevent the onset of Alzheimer’s, but the amount involved will be very small and unlikely to counteract any of the known risks of enjoying an ale.
By all means raise a glass in honour and appreciation of this research if you so desire, but don’t be seduced into thinking you’re improving your health as you do so!
Is beer really to blame for that belly?
There is no level of alcohol intake that confers any actual benefits on your health. Notwithstanding that revelation, the fact remains that a vast number of Australians continue to drink at least in moderation. With that in mind, one pertinent question among moderate drinkers might be, are some alcoholic drinks more likely to affect your waist size than others?
The answer, it seems, is yes. Research suggests that some alcoholic drinks are more likely than others to contribute to an increase in levels of visceral fat. A study published in last year revealed how different alcohol types (beer/cider, red wine, white wine, sparkling, spirits) affected body composition. It found that visceral adiposity, in simple terms, too much visceral fat, varied depending on the type of alcohol consumed. Visceral fat, also often described as ‘hidden fat’, is considered to be the most damaging type of fat. It can build up around and between organs and is associated with an increased risk of cardiovascular disease, metabolic syndrome and other health complications. Typically in humans, visceral fat comprises about 10 per cent of all body fat, but an expanding waistline could be a sign that your visceral fat level has exceeded a healthy norm.
For women, a waist circumference of 80 centimetres or higher is considered to contribute to an elevated risk of a number of chronic diseases. In men, the equivalent figure is 94 centimetres. Any more than that and there’s a fair chance of seeing what is classically referred to as a ‘beer gut’.
Which takes us back to the all-important question: which alcoholic drinks are more likely to give you a bigger belly? Has beer been unfairly maligned as the culprit? Yes – and no. While beer is indeed a contributor to elevated levels of visceral fat, it is not the only one. Spirits fall into the same category. If you’re planning to continue enjoying a tipple but want to keep your waist expansion to a minimum, wine is your best bet and if you prefer a pinot noir to a pinot grigio, the news is better still. Red wine has actually been linked to lower levels of visceral fat. That’s not to say red wine is beneficial for your health, but, if you are going to have a drink, then a drop of red gives you a greater chance of keeping your waistline within a healthy range.
If you don’t place too much importance on body shape, does any of this really matter? Yes, because of the clear links between an oversized waistline and chronic health problems. By all means enjoy your drink of choice, but keep in mind the risks that enjoyment entails.
What does being drunk actually do to your body?
Many of us know what it feels like to wake up with a sore head after one too many drinks, but have you ever wondered what being intoxicated actually does to your body? Here are some of the physical and mental effects of overindulging in alcohol.
Health risks.
Even though some types of alcoholic beverages, such as red wine, contain antioxidants, the negative impact of alcohol outweighs its positive effects. To reduce the risk of harm from alcohol-related disease or injury, healthy men and women should drink no more than 10 standard drinks a week and no more than four standard drinks on any one day. The less you drink, the lower your risk of harm from alcohol.
Drinking an excessive amount of alcohol increases the risk of cancer and cardiovascular diseases and can also raise your blood pressure and be harmful to all organs in your body, including the stomach and liver. Excessive drinking is damaging to the liver in two big ways, the first being a type of scarring called cirrhosis. Scar tissue builds up because alcohol changes the chemicals that break down and remove scar tissue, over time, this means scar tissue replaces healthy cells and the liver struggles to work properly.
Alcohol can cause a build-up of fat in the organ: Fatty liver disease can stop it from working properly. This is reversible in the first instance, by stopping alcohol consumption for [at least] two weeks. The calorific nature of alcohol means that the body also uses this as an energy source while fat is stored, drinking excessively can lead to weight gain – and for men especially this gathers around the belly, which is a risk factor for cardiovascular disease.
As well as the direct impact, drinking to the point of intoxication can contribute to other health issues and it increases the risk of injuries and contagious diseases, especially respiratory diseases.”
Brain activity.
While knocking back drinks might bring feelings of euphoria and an initial burst of energy, it’s a different story in your grey matter. Drinking alcohol affects our central nervous system and slows down brain activity as well as affecting our memory and self-control. That’s why some people engage in more risky behaviour while drunk – or perhaps they fall over, and can’t remember how they got those bruises the next morning.
Sleep problems.
If you have trouble sleeping, alcohol might seem to help in the short term, as it can make you feel more relaxed but regularly drinking alcohol can make sleep problems worse and even if you’re conked out after a few drinks, the sleep you’re getting isn’t as good. Alcohol can impair the restorative part of the sleep cycle, REM, as well as interfering with the flow of calcium into nerve cells, affecting the region of the brain that controls sleep function. You may find yourself waking up more frequently, too:
Alcohol also causes dehydration – it inhibits the anti-diuretic hormone (ADH) causing you to use the toilet more regularly.
Emotional effects.
Alcohol can alter our moods. While having a couple of drinks can cause a spike of dopamine, which induces the ‘happy drunk’ feeling, in the long-run alcohol can act as a depressant. Regularly drinking alcohol affects your brain chemistry in a way that can lead to feelings of depression which can create a damaging cycle.
People may drink alcohol because they feel depressed, but heavy use depresses their mood further, which leads to more drinking, and so on.
|
||
|
|
||
|
|
||
|
Back Go to page: 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Forward |
||