
|
Vol 71 |
Page 11 |
Privacy Policy | Editorial Policy | Profit Policy | Join the Association | List of Members | Contact us | Index | Links
Back Go to page: 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Forward
Veterans and Veterans Families Counselling Service (VVCS) can be reached 24 hours a day across Australia
for crisis support and free and confidential counseling. Phone 1800 011 046.
VVCS is a service founded by Vietnam Veterans.

Health and Life-style.
Contents.
Anti-depressants and their side effects.
Corona virus - long term effects.
Diet changes for women over 50.
Goosebumps - why do we get them.
Sex problems:
Erectile dysfunction drugs and high blood pressure.
High blood pressure challenges.
COVID-19 (coronavirus): Possible Long-term effects.
COVID-19 symptoms can sometimes persist for months. The virus can damage the lungs, heart and brain, which increases the risk of long-term health problems.
Most people who have coronavirus disease 2019 (COVID-19) recover completely within a few weeks, but some people — even those who had mild versions of the disease — continue to experience symptoms after their initial recovery.
Older people and people with many serious medical conditions are the most likely to experience lingering COVID-19 symptoms. The most common signs and symptoms that linger over time include:
-
Fatigue
-
Cough
-
Shortness of breath
-
Headache
-
Joint pain
Although COVID-19 is seen as a disease that primarily affects the lungs, it can damage many other organs as well. This organ damage may increase the risk of long-term health problems. See the video below.
Organ damage caused by COVID-19
Organs that may be affected by COVID-19 include:
-
Heart. Imaging tests taken months after recovery from COVID-19 have shown lasting damage to the heart muscle, even in people who experienced only mild COVID-19 symptoms. This may increase the risk of heart failure or other heart complications in the future.
-
Lungs. The type of pneumonia often associated with COVID-19 can cause long-standing damage to the tiny air sacs (alveoli) in the lungs. The resulting scar tissue can lead to long-term breathing problems.
-
Brain. Even in young people, COVID-19 can cause strokes, seizures and Guillain-Barre syndrome — a condition that causes temporary paralysis. COVID-19 may also increase the risk of developing Parkinson's disease and Alzheimer's disease.
Blood clots and blood vessel problems
COVID-19 can make blood cells more likely to clump up and form clots. While large clots can cause heart attacks and strokes, much of the heart damage caused by COVID-19 is believed to stem from very small clots that block tiny blood vessels (capillaries) in the heart muscle.
Other organs affected by blood clots include the lungs, legs, liver and kidneys. COVID-19 can also weaken blood vessels, which contributes to potentially long-lasting problems with the liver and kidneys.
Problems with mood and fatigue.
People who have severe symptoms of COVID-19 often have to be treated in a hospital's intensive care unit, with mechanical assistance such as ventilators to breathe. Simply surviving this experience can make a person more likely to later develop post-traumatic stress syndrome, depression and anxiety.
Because it's difficult to predict long-term outcomes from the new COVID-19 virus, scientists are looking at the long-term effects seen in related viruses, such as severe acute respiratory syndrome (SARS).
Many people who have recovered from SARS have gone on to develop chronic fatigue syndrome, a complex disorder characterized by extreme fatigue that worsens with physical or mental activity, but doesn't improve with rest. The same may be true for people who have had COVID-19.
Many long-term COVID-19 effects still unknown
Much is still unknown about how COVID-19 will affect people over time. However, researchers recommend that doctors closely monitor people who have had COVID-19 to see how their organs are functioning after recovery.
It's important to remember that most people who have COVID-19 recover quickly. But the potentially long-lasting problems from COVID-19 make it even more important to reduce the spread of the disease by following precautions such as wearing masks, avoiding crowds and keeping hands clean.
![]()
Goosebumps – why do we get them?
Goosebumps may help protect animals in the cold, but Harvard University researchers found there’s a different reason humans evolved this reaction.

Stop it, you’re giving me Goosebumps. Sometimes a compliment, sometimes a warning signal. Always a mystery.
Well, until now.
Science has had its day and finally uncovered just why it is we get Goosebumps. Sure, we know when they appear, when we’re cold, we’re in a heightened emotional state and for some people, when they’re on the toilet. It’s known that Goosebumps are a throwback to our hairier days, when cold temperatures would signal our body to bristle our human-coats to keep us warm.
In scientific terms, the sympathetic nerve in our skin contracts in the cold, pulling a wee muscle that’s connected to the bottom of a hair follicle. This makes the hair stand up on end, while simultaneously bringing the skin around its base inwards, creating a little bump.
The skin is a fascinating system: It has multiple stem cells surrounded by diverse cell types, and is located at the interface between our body and the outside world, therefore, its stem cells could potentially respond to a diverse array of stimuli – from the niche, the whole body, or even the outside environment.
When it’s cold the muscle in the hair follicle contracts, creating Goosebumps. The sympathetic nerve also releases neurotransmitters to stem cells in the hair follicle.
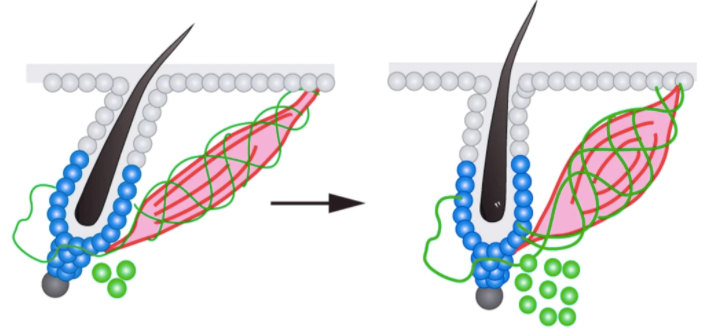
Harvard Uni used electron microscopy to examine the skin, focusing on the sympathetic nerve. They found that nerve also connect to the stem cells of the hair follicle, so when it does its cold contract-dance, the stem cells are pushing into gear to grow a new hair.
What does that mean? It means Goosebumps act to not only spring into action the hair that we do have (or had) to keep us warm, but tell our body to grow more hair, to keep us even warmer. This particular reaction is helpful for coupling tissue regeneration with changes in the outside world, such as temperature. It’s a two-layer response, Goosebumps are a quick way to provide some sort of relief in the short term, but when the cold lasts, this becomes a nice mechanism for the stem cells to know it’s maybe time to regenerate new hair coat.
Oh - and why are they called Goosebumps?
Because they look like the feather-less skin of a goose, or similar poultry.
First time in history – we can save the human race by laying in front of the TV and doing nothing.
Let’s not screw this up!
Simple steps for cutting sugar from your diet.
Eating too many sweets can lead to a variety of health problems. To curb your consumption, start by getting smarter about the sources of sugar in your diet.
Craving sweets from time to time is natural. Too much sugar in your diet, however, increases the risk of weight gain, elevated triglycerides, poor nutrition and tooth decay. The World Health Organization recommends that both adults and children keep their intake of added sugars to less than 10 percent of daily calories (about 12 teaspoons of sugar). To get a handle on your sugar intake, it's important to become aware of the sources of sugar in your diet.
Start by reading food labels. Sugar goes by many aliases, including corn syrup, molasses, honey, high-fructose corn syrup, malt sugar and dextrose. Understand that natural sugar occurs in foods such as fruit, milk and plain yogurt. Added sugar is added to foods or beverages, either in processing (as in soda and flavoured yogurt) or in preparation (as when you add sugar to coffee). Recommendations about sugar consumption don't include foods with naturally occurring sugars because those foods usually contain other beneficial nutrients, such as vitamins, minerals, fibre and protein.
Other helpful tips for cutting sugar consumption in your diet include:
-
Investigate the sugar content of your favourite food. Minimize the amount of added sugar in your food selections and be on the lookout for sweeteners.
-
Buy and eat fewer processed foods. Purchase more whole foods, including fruits, vegetables and whole grains, and experiment with new recipes.
-
Change your environment. Exchange the candy bowl at work or at home with a fruit bowl.
Sexual Health - Do natural aphrodisiacs actually work?
There's little evidence to support the effectiveness of most substances thought of as natural aphrodisiacs, natural substances that may enhance sexual function. Some foods and supplements are sometimes claimed to affect libido, these include chocolate, spicy food and saw palmetto, but research has found that they usually don't work to produce a sexual response in men or women.
The pursuit of remedies or substances that enhance sexual pleasure has been a human obsession for millennia. The 18th-century cad Casanova reportedly consumed a few-dozen oysters daily for breakfast to increase his libido, while Cleopatra favoured saffron to lure her lovers. The ancient Indian sex guide the Kama Sutra encouraged lovers to anoint their private parts with honey and black pepper (ouch).
Some modern (early) evidence is a little more encouraging for a few natural supplements, but more research is needed. These include ginkgo, ginseng, maca and tribulus.
There's no harm in trying most foods to see if they're effective natural aphrodisiacs, but be aware that some supplements that have insect or plant extracts in them can be poisonous (toxic). For example, Spanish fly, a commonly advertised natural aphrodisiac, can cause kidney damage and bleeding in the digestive system.
Certain products sold as natural aphrodisiacs have also been found to include prescription drug ingredients that aren't listed on the label. For example, sildenafil, the active ingredient in Viagra, has been found in some products. These ingredients can be dangerous if you have certain medical conditions or take certain drugs.
Aphrodisiacs – the phrase originates from the Greek goddess of love and sexuality, Aphrodite, are thought to work in one of two ways: by arousing the mind or by stimulating other parts of the body such as increasing blood flow in the sex organs.
If you're looking for a way to increase your sexual desire that can work, talk to your doctor. He or she may suggest proven strategies for enhancing sexual health. These may include communicating with your partner, making healthy lifestyle choices and treating any other medical conditions you have. You may also find it helpful to talk to a counsellor or therapist trained in sexual concerns and relationship issues.
Antidepressants – and their side effects.
Sexual side effects are common with antidepressants in both men and women, these effects can include:
-
A change in your desire for sex
-
Erectile problems
-
Orgasm problems
-
Problems with arousal, comfort and satisfaction
The severity of sexual side effects depends on the individual and the specific type and dose of antidepressant. For some people, sexual side effects are minor or may ease up as their bodies adjust to the medication. For others, sexual side effects continue to be a problem.
Antidepressants with the lowest rate of sexual side effects include:
-
Bupropion (Wellbutrin XL, Wellbutrin SR)
-
Mirtazapine (Remeron)
-
Vilazodone (Viibryd)
-
Vortioxetine (Trintellix)
Antidepressants most likely to cause sexual side effects include:
-
Selective serotonin reuptake inhibitors (SSRIs), which include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil, Pexeva) and sertraline (Zoloft).
-
Serotonin and norepinephrine reuptake inhibitors (SNRIs), which include venlafaxine (Effexor XR), desvenlafaxine (Pristiq) and duloxetine (Cymbalta).
-
Tricyclic and tetracyclic antidepressants, such as amitriptyline, nortriptyline (Pamelor) and clomipramine (Anafranil).
-
Monoamine oxidase inhibitors (MAOIs), such as isocarboxazid (Marplan), phenelzine (Nardil) and tranylcypromine (Parnate). However, selegiline (Emsam), an MAOI that you stick on your skin as a patch, has a low risk of sexual side effects.
If you're taking an antidepressant that causes sexual side effects, your doctor may recommend one or more of these strategies:
-
Waiting several weeks to see whether sexual side effects get better.
-
Adjusting the dose of your antidepressant to reduce the risk of sexual side effects. But always talk with your doctor before changing your dose.
-
Switching to another antidepressant that may be less likely to cause sexual side effects.
-
Adding a second antidepressant or another type of medication to counter sexual side effects. For example, the addition of the antidepressant bupropion may ease sexual side effects caused by another antidepressant.
-
Adding a medication to improve sexual function, such as sildenafil (Viagra), tadalafil (Cialis) or vardenafil (Levitra, Staxyn). These medications are approved by the Food and Drug Administration only to treat sexual problems in men. Limited research suggests that sildenafil may improve sexual problems caused by antidepressants in some women, but more information is needed on its effectiveness and safety in women.
Stopping medication because of sexual side effects is a common problem, and for most people this means depression returns. Work with your doctor to find an effective antidepressant or combination of medications that will reduce your sexual side effects and keep your depression under control.
If you're pregnant or trying to become pregnant, tell your doctor, as this may affect the type of antidepressant that's appropriate.
Be patient. Everyone reacts differently to antidepressants, so it may take some trial and error to identify what works best for you.
High blood pressure and sex: Overcome the challenges
High blood pressure often has no signs or symptoms, but the impact on your sex life may be obvious. Although sexual activity is unlikely to pose an immediate threat to your health, such as a heart attack, high blood pressure can affect your overall satisfaction with sex.
A link between high blood pressure and sexual problems is proved in men. For women who have decreased sexual satisfaction, it's not yet proved that high blood pressure is to blame.
Over time, high blood pressure damages the lining of blood vessels and causes arteries to harden and narrow (atherosclerosis), limiting blood flow. This means less blood is able to flow to the penis. For some men, the decreased blood flow makes it difficult to achieve and maintain erections, often referred to as erectile dysfunction. The problem is fairly common. High blood pressure can also interfere with ejaculation and reduce sexual desire. Sometimes the medications used to treat high blood pressure have similar effects.
Even a single episode of erectile dysfunction can cause anxiety. Fears that it will happen again might lead men to avoid sex and affect the relationship with their sexual partner.
Men should discuss any concerns with their doctor.
High blood pressure's effect on sexual problems in women isn't well-understood. But it's possible that high blood pressure could affect a woman's sex life. High blood pressure can reduce blood flow to the vagina. For some women, this leads to a decrease in sexual desire or arousal, vaginal dryness, or difficulty achieving orgasm. Improving arousal and lubrication can help.
Like men, women can experience anxiety and relationship issues due to sexual dysfunction. Women should talk to their doctor if they experience these difficulties.
High blood pressure medications that can cause sexual dysfunction as a side effect include:
-
Water pills (diuretics). Diuretics can decrease forceful blood flow to the penis, making it difficult to achieve an erection. They can also deplete the body of zinc, which is necessary to make the sex hormone testosterone.
-
Beta blockers. These medications, especially older generation beta blockers such as propranolol (Inderal, Innopran XL), are commonly associated with sexual dysfunction.
To reduce the risk of side effects from these medications, including sexual problems, take medications exactly as prescribed. If you still have side effects, talk to your doctor about other possible medications that may have fewer side effects.
If sexual side effects persist, ask your doctor about other medication options. Some high blood pressure medications are less likely to cause sexual side effects, such as:
-
Angiotensin-converting enzyme (ACE) inhibitors
-
Calcium channel blockers
-
Angiotensin II receptor blockers
To help your doctor select the most appropriate medication for you, tell him or her all the other medications you're taking now, including herbal supplements and over-the-counter drugs. Sometimes a particular combination of medications or supplements contributes to sexual problems.
If your doctor says it's OK, you may be able to stop taking blood pressure medications temporarily to see if your sex life improves. To make sure your blood pressure remains within a safe range, you may need frequent blood pressure readings while you're not taking the blood pressure lowering medication that may be causing your sexual difficulties. This can be done with a home blood pressure monitoring device for convenience.
Erectile dysfunction drugs and high blood pressure.
Men considering medications for erectile dysfunction should check with their doctor first. It's usually safe to combine the erectile dysfunction drugs sildenafil (Revatio, Viagra), vardenafil (Levitra, Staxyn) and tadalafil (Adcirca, Cialis) with high blood pressure medications.
Taking these drugs with nitrates, taken either regularly for chest pain or in an emergency setting, can cause a dangerous drop in blood pressure. If you have high blood pressure, you usually don't have to live with a loss of sexual satisfaction. The more your doctor knows about you, the better he or she can treat your high blood pressure and help you maintain a satisfying sex life. Be prepared to answer questions your doctor may ask, such as:
-
What medications are you taking?
-
Has your relationship with your sexual partner changed recently?
-
Have you been feeling depressed?
-
Are you facing more stress than usual?

By making healthy lifestyle choices, you can lower your blood pressure and potentially improve your sex life. Healthy lifestyle choices include:
-
Not smoking or using tobacco
-
Eating healthy foods
-
Limiting alcohol consumption
-
Reducing the amount of salt in your diet
-
Losing extra pounds
-
Exercising regularly
Of course, a leaner body can boost your confidence and help you feel more attractive, which could also improve your sex life.
Your sexual response may vary with feelings about your partner and the setting in which sex occurs. To encourage satisfying sex, initiate sex when you and your partner are feeling relaxed. Explore various ways to be physically intimate, such as massage or warm soaks in the tub. Share with each other the types of sexual activity you enjoy most. You may find that open communication is the best way to achieve sexual satisfaction.
Diet changes women over 50 should make right now.
Your body changes as you age, so your diet needs to change, too. These tips from a Mayo Clinic wellness dietitian can help ensure you're getting the nutrients you need.
You are what you eat, right? For women over 50, eating the right foods becomes even more important to avoid health problems. It is suggested that women over 50 target three important nutrients to combat the most common changes caused by aging.
1. Calcium for bone health
Osteoporosis gets a fair amount of attention and most older women understand that the risk of developing this bone disease increases with age. In fact, 1 in 3 women over 50 is at risk of a bone break caused by osteoporosis. Osteoporosis affects men, too, but not at such high rates. Women absorb less calcium as they age, and some women's ability to tolerate dairy, the best sources of calcium, also decreases as they get older. Dark leafy greens and calcium-fortified orange juice are other good sources.
Women over 50 need 1,200 milligrams of calcium daily. Use the Nutrition Facts label on food products to keep track of your intake.

2. Protein for healthy muscle mass
Older women tend to sit more, exercise less. That compounds a natural aging process called sarcopenia, which is the loss of muscle mass. By the time women near 80 years, they may have lost as much as half of their skeletal muscle mass. Eating enough protein reduces the impact of that muscle wasting. Healthy plant-based diets that don't include meat, a major source of protein, can still provide plenty of protein if you make savvy choices, choose more soy, quinoa, eggs, dairy, nuts, seeds and beans. Your protein needs depend on how much you weigh. For women over 50, experts recommend 1 to 1.5 grams of protein per kilogram of weight. If you weigh 75kg, for instance, you would need at least 115 grams of protein a day.
3. Vitamin B-12 for brain function
As women age, they absorb fewer nutrients from their food. One key nutrient they may not be absorbing enough of is vitamin B-12, which is essential for maintaining both healthy red blood cells and brain function. The best sources of vitamin B-12 are eggs, milk, lean meats, fish and fortified foods like cereals and grains. Vegans, in particular, will need to choose more fortified foods, but even elderly people who eat all foods may have difficulty absorbing enough vitamin B-12.
While the recommended daily intake of vitamin B-12 for women over 50 is 2.4 micrograms a day, you should talk with your doctor to see if you also need a supplement. The three tips to help women over 50 get the nutrition they need are:
-
Make whole foods the foundation of your diet. Focusing on whole grains, fruits and veggies will help avoid a lot of common problems that come with age.
-
Drink before you're thirsty. The way your body detects thirst changes as you age, make sure to drink plenty of water, even if you don't feel thirsty. Carry a water bottle and drink a glass with every meal.
-
Make an appointment with food. (And keep it.) Create concrete plans that lay out exactly how you’ll get key nutrients. Write the plan on a calendar. By simply making an 'appointment' with that apple, you're more likely to eat it.
Losing weight doesn’t seem to be working for me
so I’m going to concentrate on getting taller.
Fragile or thin skin that tears easily is a common problem in older adults. Aging, sun exposure and genetics all play a role in thinning skin. Certain medications, such as long-term use of oral or topical corticosteroids (used to treat a wide variety of disorders, including asthma, arthritis, skin conditions and autoimmune diseases), also can weaken the skin and blood vessels in the skin. Thin skin isn't necessarily a sign of a serious underlying medical condition. But you might want to see a doctor, who can evaluate your skin.
To protect thin skin and prevent tears and cuts:
-
Wear long-sleeved shirts, long pants and wide-brimmed hats. Consider wearing two layers to protect your forearms when doing yard-work or gardening, common areas for minor injury to the skin. You might also try wearing tubular or rolled gauze bandages.
-
Avoid prolonged sun exposure.
-
If you must be outside in the sun, use a water-resistant, broad-spectrum sunscreen with an SPF of at least 30. Apply sunscreen generously and reapply every two hours — or more often if you're swimming or sweating.
-
Keep skin well-moisturized and protected by using a good moisturizing cream.
-
Talk to your doctor about treating skin with vitamin A (retinol), which might improve your skin's ability to tolerate injuries.
A new and easy self-test for the horror of Covid 19 is doing the rounds and it's simple, quick and positive (or negative if you see what I mean). Take a glass and pour a decent dram of your favourite whisky into it (it may also work with other spirits but I am yet to try them); then see if you can smell it. If you can, then you are halfway there.
Then drink it. If you can taste it then it is reasonable to assume you are currently free of the virus because the loss of the sense of smell and taste is a common symptom.
I tested myself 7 times last night and was virus free every time thank goodness. I will have to test myself again today because I have developed a throbbing headache which can also be one of the symptoms.
I'll report my results later.
Back Go to page: 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Forward